How to Fill Out SOAP Note Examples
The SOAP note examples are generally used in hospital or other kind of health center. It is specific document where the health officer can record patient’s information during treatment process. The document supplementary will be gathered to the main medical record for each patient. Another purpose of the document is that other health practitioners who also handle the patient will be informed well about their conditions.
There are many formats of SOAP note examples which are generally utilized by specialists in health sector. The document becomes likely evidence that the patient has been through clinical assessment. Based on the reasoning from the note, the professionals will provide the next measurements needed.
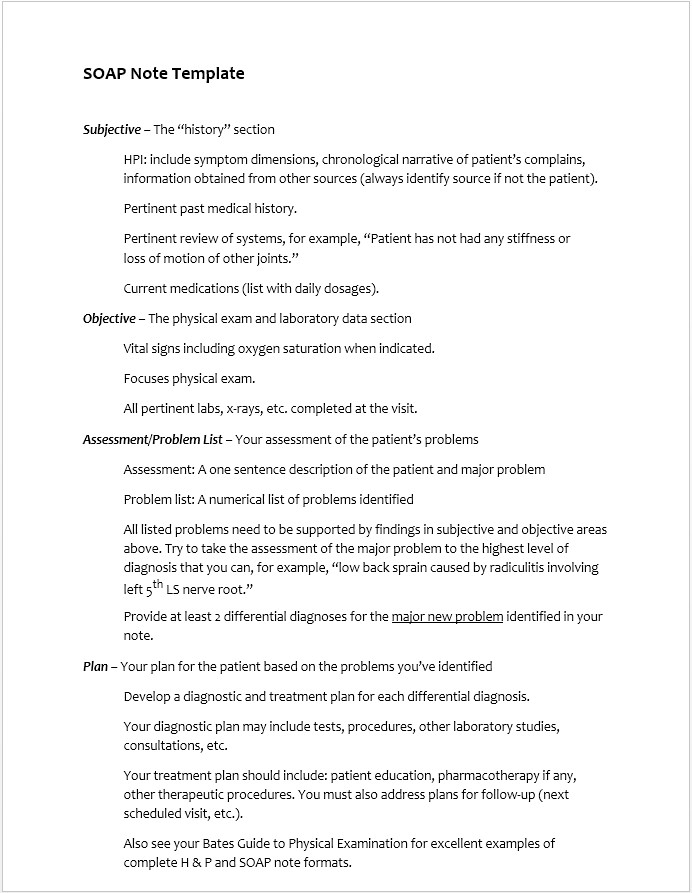
- Filling out the S
S from SOAP note examples stands for Subjective. The information put on subjective is gathered from patients themselves. The health care providers should ask their patient to describe what conditions concerns them. Through their narration, the professionals will be able to discover their problems including disabilities, symptoms, functions and their history.
The health care provider should be able to catch only the relevant information about present condition. You should also avoid giving them questions that only have to be answered with yes or no. Also, you are not allowed to judge the patient to be overreacting as it will help you to move on the next step when you try to determine exact potential disease.
- Filling out the O
O is Objective section from the SOAP note examples. After the patient, now it’s the professionals turn to give write their observation. This is more measurable since you will use some tools as intervention and see how the patient responds. Through those examination, you can write the results on measurements including frequency, duration along with the equipment.
The examination could be blood circulation, range of motion, vision, palpation and simple muscular tests. If you need to do some special tests, then you have to highlight it properly at the note. Provide this information in details as much as possible along with the identified injuries.
- Filling out the A
A from SOAP note examples is described as assessment. The professional health care should withdraw their opinion based on the subjective and objective sections. You should also explain why the chosen measurements are the best among the others. The explanation should state the patient progress as well as negative factors that could affect the treatment.
- Filling out the P
P stands for plan where it contains all interventions that patient should be through. This would be including medication, surgeries and therapies. Although most of them are short term measurements, you can also include the long term plan where you usually suggest your patient to change the lifestyle.
Soap Note Examples
Soap Note Examples for Nurse Practitioners
Soap note examples for occupational therapy
Soap Note Examples Mental Health

The content creator team at calipsotree.com is dedicated to making topics accessible to everyone, with over 9 years of experience in writing and breaking down complex concepts into easy-to-understand articles that answer readers’ financial questions.